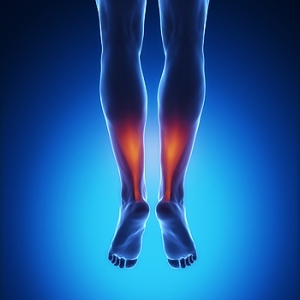
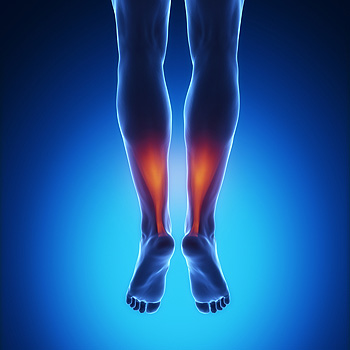
Symptoms Of An Achilles Tendon Injury
The Achilles tendon connects the heel to the calf muscles, and it is located in the back of the leg, directly above the heel. It is known to be the largest tendon in the body, and if it should become injured, it may be difficult to walk and run. This tendon enables the foot to point and flex, in addition to standing on tiptoe. There are noticeable symptoms that exist if an Achilles tendon injury has occurred. These can include severe pain in the back of the leg, the inability to bend the foot, and some patients may also notice the ankle is bruised and weak. As the aging process occurs, it is important to perform proper stretches that can keep the Achilles tendon strong, and this may be helpful in preventing a painful injury from occurring. It can become torn or injured if you suddenly step off of a curb, which may overstretch the tendon. Moderate relief may be found when the affected foot is elevated, and it may feel comforting if an elastic bandage is wrapped around the foot to provide additional support. If you have injured your Achilles tendon, it is advised that you consult with a podiatrist who can properly treat this condition.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Milos Tomich, DPM of Dr. Tomich Foot & Ankle Health Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Milwaukee and Wauwatosa, WI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
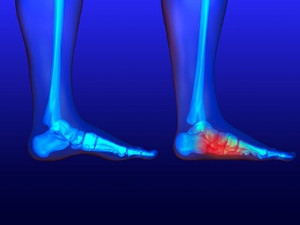
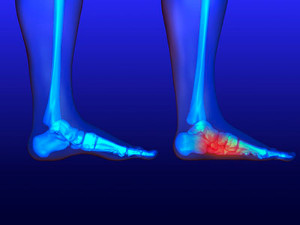
Repetitive Motions and Stress Fractures
 The causes of stress fractures often include an injury to the bone that has occurred from overuse. Research has indicated the feet may endure approximately twelve times the weight of the body as each step is taken. The symptoms that are most often noticed are pain while walking or running, in addition to swelling and tenderness. Stress fractures are commonly caused by repetitive motion that may come from participating in running and jumping activities. If the injury is treated when the symptoms are first noticed, mild relief may be found when the affected foot is elevated, and the activity that caused the injury is ceased. For more severe stress fractures, it is advised that you seek the counsel of a podiatrist who can properly diagnosis and treat stress fractures.
The causes of stress fractures often include an injury to the bone that has occurred from overuse. Research has indicated the feet may endure approximately twelve times the weight of the body as each step is taken. The symptoms that are most often noticed are pain while walking or running, in addition to swelling and tenderness. Stress fractures are commonly caused by repetitive motion that may come from participating in running and jumping activities. If the injury is treated when the symptoms are first noticed, mild relief may be found when the affected foot is elevated, and the activity that caused the injury is ceased. For more severe stress fractures, it is advised that you seek the counsel of a podiatrist who can properly diagnosis and treat stress fractures.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Milos Tomich, DPM from Dr. Tomich Foot & Ankle Health Center. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact one of our offices located in Milwaukee and Wauwatosa, WI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Stretches for Flat Feet
 The medical condition that is referred to as flat feet is also known as fallen or collapsed arches. This can occur as a result of an injury that has happened to the foot, genetic factors, or medical reasons that may include arthritis or pregnancy. Patients may experience pain and discomfort as a result of having this ailment, and it may affect the overall alignment of the body. Research has indicated there are stretches that can be performed which may be helpful in strengthening the feet. An effective way to stretch the heel is to extend one leg behind the other. As the heels are pressing into the floor, the heels and Achilles tendon are stretched. Some patients also find that it helps to roll their feet on top of a tennis or golf ball. This may help to stretch and strengthen the plantar fascia. If you have flat feet and would like additional information about how to perform stretches, please consult with a podiatrist.
The medical condition that is referred to as flat feet is also known as fallen or collapsed arches. This can occur as a result of an injury that has happened to the foot, genetic factors, or medical reasons that may include arthritis or pregnancy. Patients may experience pain and discomfort as a result of having this ailment, and it may affect the overall alignment of the body. Research has indicated there are stretches that can be performed which may be helpful in strengthening the feet. An effective way to stretch the heel is to extend one leg behind the other. As the heels are pressing into the floor, the heels and Achilles tendon are stretched. Some patients also find that it helps to roll their feet on top of a tennis or golf ball. This may help to stretch and strengthen the plantar fascia. If you have flat feet and would like additional information about how to perform stretches, please consult with a podiatrist.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Milos Tomich, DPM from Dr. Tomich Foot & Ankle Health Center. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact one of our offices located in Milwaukee and Wauwatosa, WI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Is Hammertoe A Deformity?
There are noticeable signs you may have a hammertoe. These can include the second toe bending in a downward direction, often resembling a hammer. Additionally, it may bend over the third toe, and it may be difficult to walk. This condition may be caused by genetic traits, or can come from wearing shoes that do not have enough room for the toes to move freely in. It is considered to be a deformity of the bones in the toes, and in severe cases, surgery may be required to permanently straighten the toes. In the beginning stages of hammertoe, mild relief may be found when larger shoes are worn that can accommodate the bent toes. Some patients find it beneficial to wear pads on the top of the affected toes, and this may help to prevent corns from developing. If you are afflicted with hammertoe, it is suggested that you speak to a podiatrist who can properly treat this condition.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact Milos Tomich, DPM from Dr. Tomich Foot & Ankle Health Center. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
- Pain in the affected toes
- Development of corns or calluses due to friction
- Inflammation
- Redness
- Contracture of the toes
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions please contact one of our offices located in Milwaukee and Wauwatosa, WI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
What Are Orthotics?
 Patients who have chronic foot pain may have considered wearing orthotics. They are defined as inserts that are worn inside the shoe, and may be beneficial in controlling specific types of foot pain. Orthotics are used to redistribute the weight of the body which may be helpful in relieving pain and discomfort. Patients who choose to wear orthotics may be afflicted with rheumatoid arthritis, plantar fasciitis, and find that continually wearing these custom made inserts can provide all or partial relief. If you have a foot condition that may benefit from wearing orthotics, it is advised that you seek the counsel of a podiatrist who can properly fit you for these inserts.
Patients who have chronic foot pain may have considered wearing orthotics. They are defined as inserts that are worn inside the shoe, and may be beneficial in controlling specific types of foot pain. Orthotics are used to redistribute the weight of the body which may be helpful in relieving pain and discomfort. Patients who choose to wear orthotics may be afflicted with rheumatoid arthritis, plantar fasciitis, and find that continually wearing these custom made inserts can provide all or partial relief. If you have a foot condition that may benefit from wearing orthotics, it is advised that you seek the counsel of a podiatrist who can properly fit you for these inserts.
If you are having discomfort in your feet and would like to try orthotics, contact Milos Tomich, DPM from Dr. Tomich Foot & Ankle Health Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact one of our offices located in Milwaukee and Wauwatosa, WI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.